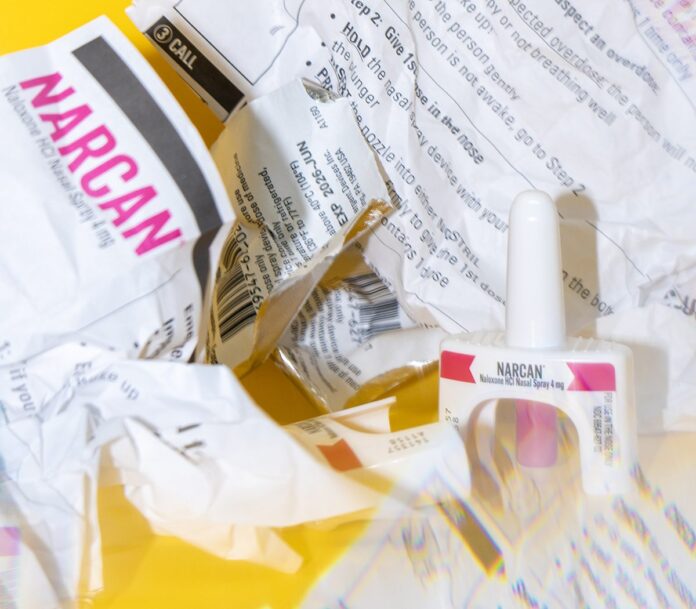
Jolt Harm Reduction in Peoria, Illinois, began in 2012 as an overdose prevention and naloxone distribution program, founded by Tamara and Blake Olt, after their 16-year-old son died from an overdose. The rural ambulance that responded to their 911 call didn’t carry naloxone, the opioid overdose reversal drug also known by the brand name Narcan.
“That could have saved his life at that moment,” said Chris Schaffner, Jolt’s executive director.
In the following years, Jolt expanded its work to include harm-reduction services like drug checking, free and sterile syringe and pipe exchanges, and sex worker outreach. Harm reduction acknowledges that, for many people, abstinence is neither possible nor desirable, and it helps people use more safely, rather than pushing them toward sobriety like many traditional recovery or treatment approaches—and it saves lives.
From 2019 until 2022, Peoria County—where Jolt is based—saw sustained decreases in fatal overdoses, while rates for Cook County and much of the country exploded. Using overdose hotspot maps, Jolt workers went door-to-door in high-risk communities and offered Narcan—and training on how to use it—to anyone who answered. Jolt, which is run by and for current and former drug users, hired queer people, people of color, and others from the communities they visited and looked for individuals and businesses to serve as focal points for continued naloxone distribution. Fatal overdoses in Peoria County decreased by 16 percent from 2020 to 2021, according to a Peoria County deputy coroner Ben Brewer. Schaffner said that the Peoria County coroner was an advocate for the work Jolt was doing. “He said that if it weren’t for harm-reduction programs distributing naloxone, we would have a significant number of deaths.”
In 2022, the last year for which data is available, 3,261 people in Illinois died from opioid overdose–related deaths. That same year, Illinois attorney general Kwame Raoul settled the first of multiple lawsuits against opioid manufacturers, dispensers, and distributors “for their unfair and deceptive practices in the marketing, sale, and distribution of these drugs,” according to the state opioid settlement website. Like the cigarette lawsuits of the 90s, these multistate suits are one attempt to hold large corporations that profited from opioid addiction and death accountable for their role in the crisis. The settlements with drugmakers and pharmacies collectively amount to billions of dollars and are divided between numerous states that were part of the lawsuits. Even so, Illinois is expected to get more than $1.3 billion by 2038. Fifty-five percent of that money will go to the Illinois Opioid Remediation Fund; the remainder is divided between state and local governments.
Most, though not all, decision-making powers for remediation funds are housed within the Illinois Department of Human Services (IDHS) and its Division of Substance Use Prevention and Recovery (SUPR). A governor-appointed steering committee determines if these funds are distributed via intergovernmental agreements, expansion of existing programs, or competitive awards. The steering committee uses Illinois’s Statewide Overdose Action Plan (SOAP) guidelines, which include five priority recommendation categories: social equity, prevention, treatment and recovery, harm reduction, and “justice-involved populations and public safety.” The goal is to reduce overdose deaths and related harms. But the half-dozen harm-reduction leaders, large nonprofit directors, psychiatrists, state lawmakers, and former IDHS workers who spoke to the Reader for this story describe a confusing and burdensome application process, promises of feedback for rejected applicants that are not delivered on, and a lack of transparency around award allocation.
“How are the opioid settlement funds working? I don’t think they’re working that well,” said state representative Lindsey LaPointe. LaPointe is the chairperson of the House Mental Health and Addiction Committee, and her remarks came the day after an October 28 hearing on the settlement funds and cannabis revenue held jointly with state senator Laura Fine, the IDHS, and harm-reduction and treatment specialists.
“It’s a boatload of money that our communities all across Illinois desperately need, and the state has been really slow to get the money out the door,” she continued. “I recognize that it’s very difficult to get public dollars out the door in the right way, but I was just stunned by how complicated the funding process is.” At least ten different boards, state departments, and other stakeholders—including members of the public, though most Illinoisans don’t know that—play some role in deciding if and how funds are spent. An unfortunate side effect of this effort to include many voices is that it obfuscates who is actually being listened to.
“I don’t know who has the most power in these decisions because it’s not something an outsider, even a legislator, can decipher,” said LaPointe. “One would probably have to sit through a bunch of meetings for six months to be able to understand that.”
In hearings and during interviews, directors of small harm-reduction organizations say they are too overburdened to successfully apply for settlement funds. Unlike large nonprofits and public health departments that have received funding so far, these community groups don’t have multimillion-dollar budgets or grant writers on staff.
“As a grassroots organization, I do not stand a chance against these bigger programs,” said Melissa Hernandez, founder of Puerto Rico Project, the first Native woman–led harm-reduction program in Illinois, at a November hearing. “I cannot afford the administrative capacity. I do not have the funds currently for these reimbursement grants.” Hernandez is a member of the low-income community she serves: She’s a former intravenous drug user and trafficking survivor. Puerto Rico Project offers showers, food, naloxone and syringes, and other core support services to housed and unhoused residents of Humboldt Park. It operates on an annual budget of $137,000. “As executive director, I’m the last to get paid—if I get paid at all.”
During the October hearing, state opioid settlement administrator Jim Wilkerson promised that a report on funds received and spent would be released sometime in November. Although the remediation fund began receiving settlement money in 2022 and “most of the work” in disbursement started in 2023 and 2024, according to Wilkerson, the report will only cover fiscal year 2024. “I think it’s very interesting to me, and somewhat disappointing, that an annual report for how we’re spending all the money doesn’t exist today,” said LaPointe later. “We’ve been doing this for almost two years. That’s just, to me, a fundamentals-of-government issue. With a funding process this complicated and this much money, that should have been part of the plan from the get-go. I’m glad it’s coming out in November.”
Midway through November, the Reader contacted IDHS for an update; spokesperson Daisy Contreras responded that the report would be out by the end of the month, but, on on December 1, I found an annual report that had been posted to IDHS’s website on November 2. I emailed Contreras to confirm whether this was the report she was referring to but, as of press time, have not received an answer.

Thanks to the continuously polluted drug supply, 2023 saw a significant increase in overdose deaths in Peoria. In 2024, Jolt applied for two Notices of Funding Opportunities (NOFO), the competitive method with which remediation funding can be dispersed. NOFOs are handled by Advocates for Human Potential (AHP), the private business contracted by IDHS to support Wilkerson, the opioid settlement administrator. AHP is tasked with writing NOFOs, reviewing and scoring applications, awarding funds, ensuring the public settlement dashboard is updated and accurate, and something called “regional coalitions coordination.”
One of the NOFOs to which Jolt applied provided funds to run harm-reduction education for youth and young adults. The other was for warm handoffs, a process that connects people with histories of substance use disorders directly to social services as they exit jails, hospitals, or shelters. “We’re already doing a lot of that work,” explained Schaffner to me this summer. “We’re trying to get some of that money just to pay my staff for the work that our other grants don’t pay for.”
Jolt was rejected from both. “I submitted one request for further information and never heard a word back from anyone,” wrote Schaffner over email in November. He and leaders of other organizations that were rejected say that feedback has been minimal, formulaic, or nonexistent. In Chicago, the harm-reduction organization Chicago Recovery Alliance (CRA) also applied for and was rejected from two NOFOs: one to run an intramuscular (IM) naloxone hub and another for community outreach and recovery support services. CRA executive director John Werning appealed their IM naloxone hub rejection and requested feedback on both their applications. The feedback he received was vague and suggested the organization answer questions that, in some cases, the CRA had thoroughly answered in its initial application.
It’s unclear if the independent appeals reviewer works for AHP or a different organization, or what their credentials are. I sent an email to Contreras asking for clarity on this but have not received a response.
A committee of at least three people with “relevant subject matter expertise, and including persons with lived experience” conducts the merit-based reviews of applications to determine how and where millions of dollars will be spent, according to the opioid settlement dashboard website. At the October hearing Wilkerson said reviewers are both AHP staff and outside “subject matter experts,” depending on the NOFO. “AHP subcontracts with people outside of their organization, so it is their responsibility,” Wilkerson explained, “but they aren’t necessarily the ones that are doing the full merit-based review.”
Is it the same three reviewers every time? Who specifically is doing each full review? What are their credentials? So far, the state has been tight-lipped. In an email to Wilkerson, the Reader asked about the “qualified independent reviewer” mentioned in the appeal letter but received no answer.
“Do legislators get to know who is evaluating those NOFOs?” Representative LaPointe asked in October.
“We can get back to you and potentially give you a list of who that may be,” replied Wilkerson.
Four weeks after the hearing, LaPointe still hasn’t learned who the reviewers are. After reaching out at the end of November, LaPointe wrote, “They said the answers would come very soon, and that they want to make sure they are getting me accurate info.” In November, IDHS denied the Reader’s FOIA request seeking the same information, citing an exemption for personal information and arguing that its release could expose reviewers to outside pressure when making their decisions. The Reader’s appeal of that denial is currently pending with the attorney general’s office.
“Who is tasked at writing these NOFOs that are effectively going to be the gold standard for the state—and community organizations—to adhere to?” asked one downstate harm-
reduction director during an interview this summer. They asked not to be named out of fear they’d be denied future funding opportunities.
Even some staff members of entities that successfully applied for and received opioid settlement funds have concerns. “We need insight into AHP and SUPR decision-
making—that’s the critical accountability for these structures,” said one, who spoke on the condition of anonymity. “With the state structure now, there’s no transparency.”
Without transparency around who conducts the reviews, applicants and legislators have to take it on faith that the reviewers are independent and have the relevant expertise to fairly evaluate each application. “I still have several outstanding questions about who the ‘subject matter experts’ are that are making these decisions in partnership with AHP,” wrote one of the half-dozen lawmakers who were present at the October hearing. AHP has a satellite office in Chicago but is based in Massachusetts. “It’s unclear if they have any experience in Illinois, or if they have any understanding of the human service landscape here.”
AHP maintains a website that tracks Illinois opioid settlement fund spending and announces NOFOs. A disclaimer at the bottom of each page notes that questions about awards can be submitted through the site’s help desk. But when clicked, the page is blank except for this message: “Welcome! You can raise a request for our HelpDesk using the options provided. There’s nothing in this portal yet.”
According to Wilkerson, AHP holds technical assistance calls and helps applicants complete NOFOs. Multiple applicants I spoke with described this assistance as “just reading the NOFO out loud.” A document provided to the Reader by a NOFO awardee this fall included anonymous feedback submitted to AHP from frustrated applicants. “No response to several emailed questions and calls. Questions submitted to the HelpDesk website were not answered or updated on the FAQ on the website,” read one. Others complained of errors on application forms: wrong budgets, inconsistent word counts, and application start dates “nearly two months after the originally scheduled start date” with no notification in between.
Perhaps in response to this feedback, at the October hearing, Wilkerson announced that the state planned to release a new NOFO for an Opioid Training and Technical Assistance Center (OTTAC). According to the notice, the OTTAC will primarily focus on communities disproportionately impacted by opioid overdoses and other harms from structural racism and health inequities. At the hearing, Wilkerson said the OTTAC’s purpose is to “help the smaller organizations learn how to apply” for NOFOs, as well as provide “back-office assistance” for managing the grants.
“Would that also include if [an applicant] were denied, providing some technical assistance as to why a denial was made and feedback?” asked state representative Jackie Haas. Yes, answered Wilkerson. The OTTAC could provide recommendations on how an application could be “tweaked, changed, [or made] better for the next round.” The NOFO application closes December 9; the OTTAC should be running sometime in 2025, approximately three years after remediation funding first became available in the state.
According to the Illinois Opioid Settlements Initiative tracking page, as of August 1, 2024, the remediation fund had received about $231 million, with the first settlement received in October 2022. According to public records from IDHS, a little more than $550,000 of that was designated—but not necessarily distributed—via 14 awards in 2024. The initial approved budget for 2025 jumps significantly, to nearly $10 million designated through 42 awards. These numbers include funds distributed via NOFO only; they exclude remediation funding distributed via intergovernmental agreements—for example, the $6 million given to the Illinois Department of Corrections for the treatment of incarcerated people—or the expansion of an existing program.
From 2024 to 2025, according to IDHS, these 42 awards will be split between 34 successful NOFO applicants. They include addiction recovery and treatment nonprofits, medical groups, and county public health departments. Six applicants received two or more awards for fiscal years 2024 and 2025; except for a county health department, all are recovery and treatment providers. McDermott Center, part of Chicago-based treatment and recovery provider Haymarket, received the most grants (four) and the most funding (a little over $1.3 million).
To date, only one harm-reduction organization, Perfectly Flawed Foundation in LaSalle, has received any funding: $350,000 over 14 months for community outreach and recovery support services. Those services, according to language in the award contract, include harm reduction. But the contract Perfectly Flawed received from AHP includes a stipulation that “federal award funds” may not be used to purchase needles or syringes if it means that the people receiving them “may use illegal drugs.” But opioid settlement remediation funds come from lawsuits, not the federal government. They are not federal dollars, and thus not subject to federal restrictions that block lifesaving care. Perfectly Flawed received its contract from AHP in late June 2024. “We’re hoping to get clarity any day,” wrote Luke Tomsha, founder and director of Perfectly Flawed, over email in November.
According to Contreras, the IDHS spokesperson, none of the NOFOs awarded so far fund syringes and pipes. However, if a program is registered as a syringe service program (SSP) with the Illinois Department of Public Health “and the purchase of harm reduction supplies is consistent with the scope of a particular grant,” she wrote, “it would be possible” for those funds to be used on syringes and needles. Perfectly Flawed is a registered SSP with the state.
When combined with a lack of transparency around who ultimately is making remediation funding decisions, confusion like this—even if it stems from what might be simple paperwork mistakes—does not assuage the anxieties of applicants who stretch shoestring budgets to try and prevent overdose death in their communities every day.
“It’s very clear to me that on-the-ground, small, nimble, authentic harm-reduction organizations are endemically underfunded,” said LaPointe. “They are on the front line of the opioid epidemic, keeping people alive and building relationships with people based on trust. Those organizations deserve opioid settlement funding. As a policymaker, I don’t know exactly what the answer is, but I’m interested in finding a way for those endemically underfunded organizations to get more support so they can do the work that they do.”
In November, Representative LaPointe and Senator Fine convened a second hearing, this time on the financial and administrative barriers treatment providers and harm reduction practitioners face in Illinois. Schaffner of Jolt was invited to speak. Just that week, he began, someone Jolt served died by accidental overdose. “I come today with heaviness in my heart,” he said, along with a sense of desperation and anger. “These are preventable deaths. . . . We can make a serious positive impact on this crisis, but we lack the resources and—often—the political will to do so.”